Invited Panels
Friday, November 17 | 2:00 PM – 3:30 PM
#1: Affirmative Care Across Domains: Advancing Behavioral Health Equity
Moderator:

Donte Bernard, Ph.D., University of Missouri
Presenters:

Ashleigh Coser, Ph.D., Licensed Health Service Psychologist, Cherokee Nation Behavioral Health
Melissa Anderson. Ph.D., MSCI, UMass Chan Medical School
Alexander Wilkins, Ph.D., UMass Chan Medical School

Isha Metzger, Ph.D., Licensed Clinical Psychologist, Owner. Cultural Concepts, LLC
Susan White, Ph.D., ABPP, University of Alabama
John Pachankis, Ph.D., Yale School of Public Health
Across the lifespan, people from historically marginalized and minoritized communities experience barriers to behavioral health care access and inclusion. Care that affirms a person’s identity and lived experience, and their dignity and value within society, can promote optimal outcomes and increase therapeutic engagement. This panel will discuss a range of challenges faced by historically marginalized populations in accessing quality mental health services, as well as service delivery approaches that help mitigate barriers that reduce service access.
Panelists speak from diverse backgrounds and bring expertise across a range of domains and populations including the Deaf and Hard of Hearing community, Indigenous/ American Indian peoples, African Americans, sexual and gender minority people community, and those who identify as neurodiverse. We address issues of discrimination, generational trauma, and socialization and also how these factors intersect with mental health and affirmative treatment thereof.
Categories: Mental health disparities, Multicultural psychology, Oppression and Resilience Minority Health
Keywords: Native Americans, LGBTQ+, African Americans/Black Americans
Basic to moderate level of familiarity with the material.
Participants earn 1.5 continuing education credits
At the end of this session, the learner will be able to:
- 1. Identify barriers to service access that are both shared (across underserved groups) and unique, and key principles of CBT that are affirming.
2. Describe historical and current aspects of minoritized communities lived experience impacting access to care and be able to discuss strategies for optimizing engagement and clinical outcomes.
3. Identify community engagement strategies to address barriers via intervention development efforts, and gain exposure to completed affirming CBT interventions and those currently in the works.
Long-Term Goals:
- • Attendees will be able to identify the importance of delivering identity-affirming interventions across marginalized populations in order to overcome stigma as determinant of adverse mental health and advance mental health equity.
Outline:
- • Healing Interpersonal & Racial Trauma for Black Youth: Implications for Cognitive and Behavioral Mental Health Treatments
- The negative consequences of interpersonal trauma take a disproportionate toll on Black youth due to the compounding stress of experiencing unique race related stressors both directly and vicariously. To increase their utility in responding to and treating trauma, cognitive and behavioral therapies should integrate and address cultural risk and protective factors that are likely to influence Black families’ engagement in mental health treatment. This presentation will present research on barriers and facilitators to service utilization for Black families and describe a Learning Community for clinicians considering culture in mental health treatment for Black youth and families.
• Leveraging Community Engagement to Address Behavioral Health Disparities in the Deaf Community
- Leveraging extensive community engagement to address access barriers to traditional behavioral therapies, Dr. Anderson and Dr. Wilkins have led teams of Deaf and hearing researchers, clinicians, filmmakers, actors, artists, and Deaf people in recovery to develop and evaluate innovative treatment adaptations that are uniquely and expertly tailored for Deaf signing people. This presentation will outline our process of community-engaged intervention development, as well as showcase examples of completed interventions and interventions currently in the works.
• Working Towards Increased Access to Care and Improved Treatment Outcomes Among American Indian and Indigenous People
- Among the 574 federally-recognized American Indian (AI)/Indigenous tribes there is great diversity in beliefs, practices, and history. Historically, AIs have a low rate of service utilization and retention in behavioral health services which is often linked to several factors. Access to care, in particular specialty care like that of clinical psychology, is often quite limited within rural communities. These in combination with high prevalence rates of psychopathology and suicidal ideation warrant discussions on improved methods for engagement, retention, and enhanced outcomes for AIs. This presentation will explore factors impacting service utilization, strategies for increasing access to care, and improving treatment outcomes among AI communities.
• LGBTQ-affirmative Mental Health Care: From Theory to Trials to Community Implementation and Global Dissemination
- Sexual and gender minority (SGM) individuals experience among the highest rates of depression, anxiety, substance use problems, and suicidality of any population risk group. This presentation will review theoretical and empirical advances in psychiatric epidemiology and developmental psychopathology that identify the mechanisms through which stigma compromises SGM people’s mental health that can also serve as promising treatment targets for identity-affirming psychotherapies. The presentation will then discuss the development, application, and efficacy of the first identity-affirmative mental health intervention for SGM individuals to be tested in randomized controlled trials. The talk will conclude by examining promising studies into the implementation of this treatment within SGM-serving settings locally, nationally, and globally with the goal of reducing the barriers to identity-affirming evidence-based treatment that this population has long faced.
• Promoting Inclusion and Quality of Life for Autistic Adults
- The autistic community is a growing group of neurodiverse people spanning the full lifespan. Historically, treatments have adopted been primarily behavioral in nature, focusing on teaching skills identified by neurotypical others, such as therapists and caregivers. Though understandable in premise and often clinically supported, there is concern that such approaches do not adequately consider the autistic voice, target subjective quality of life, or embrace the value of neurodiversity. We discuss services and treatments that embrace autism and help individuals achieve personally identified goals.
Recommended Readings:
White, S. W., Schall, C., Santos, J. D., Maddox, B. B., Hillier, A., Klinger, L, & Pugliese, C. (2023). Promoting quality of life: Suggestions for mental healthcare providers working with young autistic adults. Autism in Adulthood. Doi: 10.1089/aut.2022.0106
Anderson ML, Glickman NS, Wolf Craig KS, Sortwell Crane AK, Wilkins AM, Najavits LM. Developing Signs of Safety: A Deaf-accessible counselling toolkit for trauma and addiction. Clin Psychol Psychother. 2021 Nov;28(6):1562-1573. doi: 10.1002/cpp.2596. Epub 2021 Apr 24. PMID: 33847426; PMCID: PMC8511355.
Pachankis, J. E. (2018). The scientific pursuit of sexual and gender minority mental health treatments: Toward evidence-based affirmative practice. American Psychologist, 73(9), 1207-1219.
Gone (2022). Re‐imagining mental health services for American Indian communities: Centering Indigenous perspectives. American Journal of Community Psychology, 69, 257–268. https://doi.org/10.1002/ajcp.12591
Metzger, I., Turner, E., Jernigan-Noesi, M., Fisher, S., Nguyen, J.*, Griffith, B., & Shodiya-Zeumault, S.*, (2023). Conceptualizing Community Mental Health Service Utilization for BIPOC Youth. [Special Issue] Advancing Racial Justice in Clinical Child and Adolescent Psychology, Journal of Clinical Child and Adolescent Psychology. 1-15. https://doi.org/10.1080/15374416.2023.2202236
Friday, November 17| 8:00 AM – 9:30 AM
#2: Reckoning With Our Past: An update from Behavior Therapy’s Editorial Task Force on Addressing the SOGIECE Literature
Presenters:
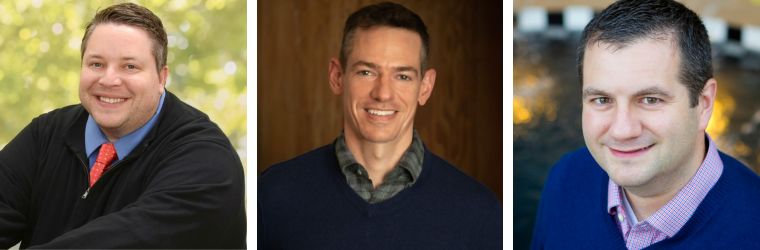
Jonathan S. Comer, Ph.D., Florida International University
John E. Pachankis, Ph.D., Yale School of Public Health
Richard T. LeBeau, Ph.D., Lyra Health

Diane Chen, Ph.D., Ann & Robert H. Lurie Children’s Hospital of Chicago, Northwestern University
David A. Langer, Ph.D., Suffolk University
Categories: LGBTQ+, Trans/Gender Health
Keywords: LGBTQ+, Sexual Minority Mental Health, Gender Minority Mental Health
Basic level of familiarity with the material
Sexual orientation and gender identity/expression change efforts (SOGIECEs) are a set of discredited and ineffective practices that pose serious risks of harm to exposed individuals. The APA and other professional governing bodies have passed clear resolutions against such so-called “conversion therapy,” and the majority of U.S. states now have prohibitory laws banning SOGIECEs.
Nonetheless, SOGIECE practices persist. As ABCT and the fields of behavioral and cognitive therapies reckon with their significant roles played in the historic development and promotion of these practices- Which continue to cause untold harms to this day– The Editor of Behavior Therapy organized a 14-member task force to collectively determine whether and what actions to take on SOGIECE articles published in the journal (i.e., “Behavior Therapy Editorial Task Force on Addressing the SOGIECE Literature”).
For this symposium, five Task Force members will provide an overview of the Task Force’s formation and missions and describe its procedural rules and decision-making thresholds. Panelists will describe the Task Force’s major discussions, debates, and deliberations, the outcomes of Task Force votes, editorial actions taken, and next steps. The symposium will conclude with opportunities for audience questions and input, and recommendations for reducing the likelihood of similar future harms to other communities.
